Fact Check: Administering Routine Medicine at Home is 12-24x Cheaper Than Hospital Care
May 12, 2025

The American healthcare system is notorious for being expensive, inconvenient, and impersonal, so it’s easy to assume that at-home medical services are financially out of reach for the average patient. But for one corner of at-home care, the cost isn’t just on par with hospital services, but 12-24x cheaper than bringing patients into a facility: routine medicine, specifically home infusion for specialty pharmaceuticals.
The financial appeal of home-based infusion is even causing a shift away from hospital care. By 2027, at-home services are expected to account for 20% of all infusions - that’s inclusive of all medicines given through an IV in hospitals, clinics, and alternate sites.
At Float, our mission is simple: to build and deploy healthcare technology that ensures the home infusion shift is a positive one for patients, pharmacists, payers, hospitals, nurses, and everyone else involved in specialty pharmaceuticals.
But you can’t control what you don’t track, so why exactly is administering routine medicine at home so much cheaper than hospital care? How can stakeholders keep costs low as the field expands?
Keep reading for a closer look at each cost-saving factor to see how they impact your corner of home infusion.
Home Infusion’s Top Cost-Saving Factors
Lower Facility Fees
Hospital facility fees and ancillary charges often account for the majority of expenses in an infusion treatment, and they’re nearly always required. But when infusion therapy is moved to the home, charges for room use, monitoring equipment, medication administration, and various other “hidden” fees are completely eliminated. Instead, patients are treated in their own environment, using equipment that’s included in the overall home infusion service package.
Depending on the treatment, patient, and hospital, removing facility fees can reduce the overall cost of treatment by up to 50%. For patients, this means smaller, or even zero, copays. The real boon is for payers, who see a drastic improvement in reimbursement payouts. In turn, everyone benefits as premiums are reduced globally.
Reduced Drug Markup Rates
Hospitals also typically apply significant markups to medications, sometimes exceeding 200-300% of the base drug cost. These inflated prices stem from hospitals’ complex pricing structures and their position in the healthcare ecosystem.
In contrast, specialty pharmacies that provide home infusion medications generally operate with much lower markup rates, often charging 20-30% less than hospitals for identical medications. The math here speaks for itself!
Fewer Re-admissions and Complications
Did you know that the CDC reports approximately 722,000 hospital-acquired infections annually, 10% of which result in death? For chronically ill and immunocompromised patients who are especially vulnerable to infections, home infusion performs an essential function: minimizing pathogen exposure.
Beyond the immediate health benefits, this reduction in complications translates to substantial financial savings by preventing costly hospital readmissions.
Additionally, home infusion therapy drives better treatment adherence rates. With non-adherance causing an estimated 40% of chronic disease treatment failures, at-home care saves the healthcare system $100B-$300B annually in avoidable expenses.
Studies Tracking Home Infusion’s Cost-Savings
Now that you know the factors behind home infusion’s financial appeal, here’s what they look like in action.
Findings from the National Home Infusion Association
A 2023 roundup review by the National Home Infusion Association examined six recent U.S. studies comparing home and inpatient infusion costs. The findings consistently demonstrated significant cost advantages for home infusion, with one particularly striking example showing anti-infective treatments costing $798 per day in a hospital setting versus just $122 per day for home infusion—a 6x cost difference.
The VA Program Case Study
A comprehensive analysis of the Veterans Affairs home intravenous antibiotic program revealed even stronger cost efficiencies. The VA program treated 98 patient courses of IV antibiotics for a total cost of approximately $610,000, while the estimated cost for the same treatments in hospital settings would have exceeded $10.8 million, driving a remarkable 17x cost difference.
Treatment Course Cost Analysis
Research published in Healthcare Journal demonstrates that home infusion therapy consistently generates savings of $1,928 to $2,974 per treatment course compared to hospital-based infusion. For patients with chronic conditions requiring regular infusions every few weeks over the course of their entire lives, these savings compound dramatically over time, potentially reducing annual treatment costs by tens of thousands of dollars per patient per annum.
From a healthcare system perspective, widespread adoption of home infusion for appropriate cases could yield tens of billions in annual savings while simultaneously improving patient experiences and outcomes.
Group Market Analysis From UnitedHealth
UnitedHealth Group’s comprehensive analysis examined comparable patients across treatment settings, controlling for various factors to isolate the true cost differential. The research ultimately found that administering specialty medications in home or office settings costs 33-52% less per month than delivering identical treatments in hospital settings.
The Top Takeaway: Revenue Opportunities Abound for Specialty Pharmacies with Perfect Adherence
Let’s return to treatment adherence. For SPs coordinating home infusion, it’s difficult to overstate just how important it is for patients to receive care on time and complete treatments in full. With non-adherence accounting for approximately 40% of chronic disease treatment failures and $100B-$300B in avoidable healthcare costs annually, gaps in compliance put a pharmacy’s bottom line at risk.
But within this risk lies potential for reward. If perfect adherence is achieved, SPs stand to gain new revenue streams, higher patient retention through improved experiences, and stronger operations.
Those improvements and more were the inspiration for Float’s AI-powered specialty pharmacy portal. Our platform empowers SPs to:
- Secure nurses for home visits in minutes
- Supply medication quickly
- Expedite reimbursements
- Reduce chart bounceback
- Monitor treatment progression
- Automates document creation
- Generate performance metrics
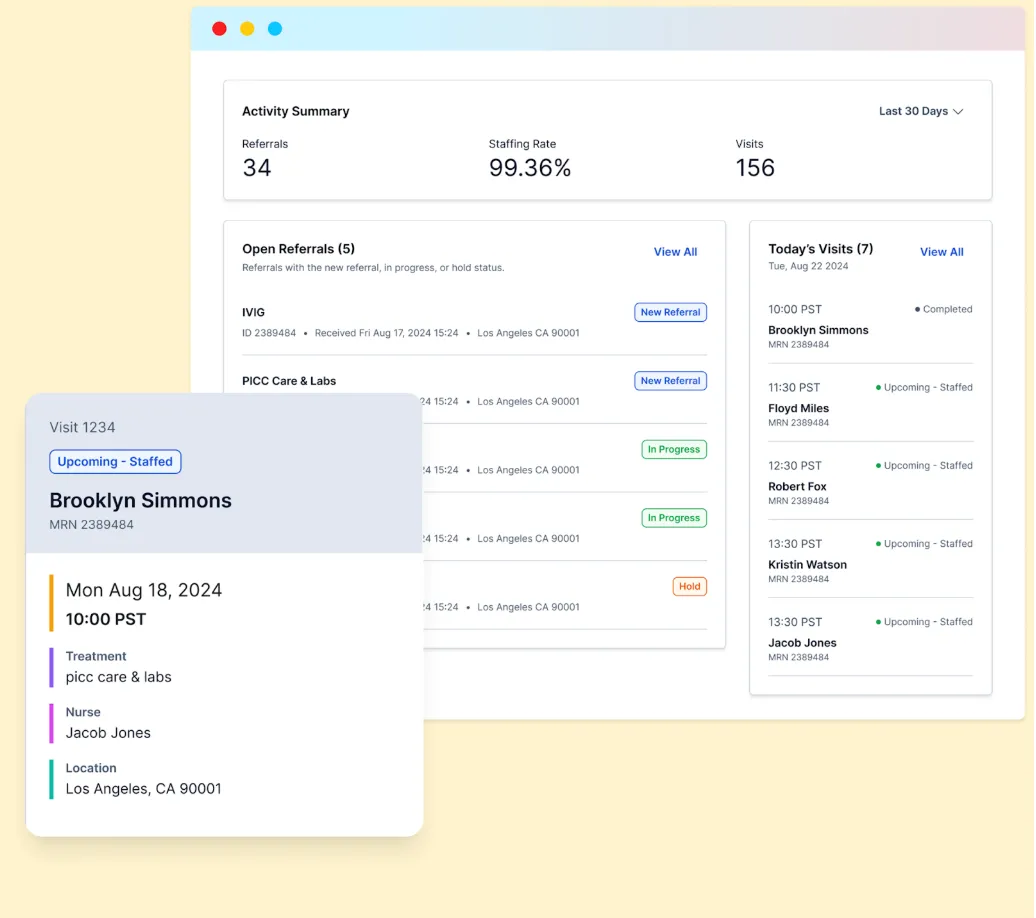
By helping SPs in their pursuit of perfect adherence, we make it possible to strengthen patient outcomes while scaling revenue per patient over time.
Additional Benefits Across the Healthcare Ecosystem
Of course, specialty pharmacies aren’t the only ones who benefit from cheaper, more streamlined care delivery.
Patients gain:
- Direct and indirect cost savings
- Quality of life improvements
- Treatment adherence benefits
Hospitals gain:
- Bed utilization optimization
- Focus on higher-acuity patients
- Resource allocation benefits
Payers gain:
- Immediate and long-term cost reductions
- Improved patient outcomes
- Better healthcare resource allocation
Real Talk: Why Isn’t Everyone Doing This Already?
Despite compelling economics, several barriers prevent wider home infusion adoption.
For one, there’s no single platform for SPs, doctors, patients, and traveling nurses to communicate. SPs must operate in a highly localized way, and it’s not uncommon for them to rely on outdated systems like Rolodexes and manual phone calls to coordinate care.
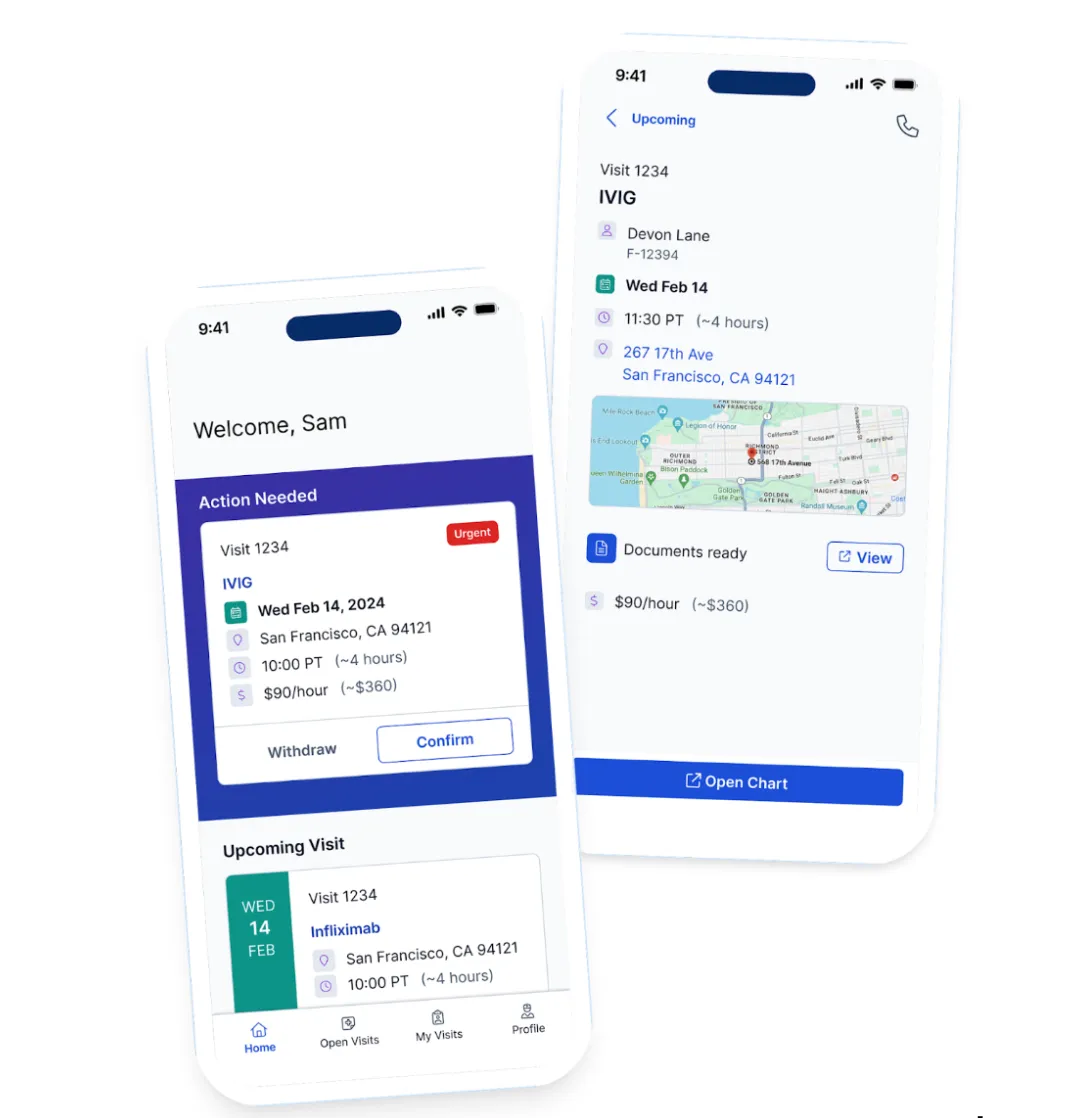
- Enter Float: Our marketplace model and SP portal matches chronic illness patients with experienced local nurses in minutes, centralizing all relevant data and info in one place for all parties to see.
Additionally, some physicians and patients have doubts about home coordination robustness. It’s simply hard to get people to trust service providers they’re unfamiliar with, and home infusion hasn’t been known historically for its care quality.
- Enter Float: While many gig-based businesses can only attract non-RNs and new RNs without other options, our unique model attracts the most experienced nurses, strengthening trust across the board.
Finally, Medicare and Medicaid reimbursement structures often don’t fully cover coordination and overhead costs, limiting provider participation. This ineffective reimbursement system prevents specialty pharmacies from being compensated for critical coordination services.
- Enter Float: We automate reimbursement for SPs, reducing working capital, accelerating RCM, and giving them better financial oversight and visibility.
Home infusion is a rare win for all parties, improving patient outcomes while delivering a 12-24x cost advantage over hospital-based care. Whether you’re a nurse seeking flexible opportunities or a pharmacy aiming to maximize adherence and revenue, join us in transforming the future of specialty pharmacy at www.FloatHealth.com.